A year after the pandemic was declared, Covid-19 continues to have devastating impacts across the world. Persistence of the virus, fresh waves of infections and the emergence of variants mean people across the world continue to live with the heart-breaking loss of loved ones, liberty and livelihoods.
Vaccines offer the best hope of a way out of the pandemic. Extraordinarily, several are already available, thanks to unprecedented global efforts and co-operation, and are being rolled out. Their effectiveness is becoming ever more evident.
The Anglican Alliance is currently working on two dimensions of the Covid-19 vaccine roll-out: advocacy on equitable global access to vaccines and sharing information to help overcome vaccine hesitancy.
Vaccine hesitancy
Most people are taking up the offer of vaccination when it becomes available, but some are hesitant.
Through the global Covid-19 task force convened by the Anglican Alliance, we have been monitoring the rollout of the vaccines and attitudes towards them. From these consultations, and a survey carried out towards the end of last year, it is clear that people are hesitant about the vaccine for two principal reasons. The first is having reasonable questions and concerns they want addressed. The second is the influence of fake news.
In two companion pieces, we explore both these areas. In part one, here, we provide information and links to answer common questions and concerns people have about the vaccines. In part two we provide a “myth-buster” section for countering fake news.
Working with the World Health Organization
The information in both pieces is from the World Health Organization. For the last few months, the Anglican Alliance has been participating in the WHO’s community of practice for faith-based organisations on Covid-19 vaccine communication.
The community of practice has been convened because the WHO recognises the key role faith communities and religious leaders are playing in the pandemic response and their importance to uptake and delivery of the vaccine(s). The WHO understands that religious leaders are trusted by the communities they serve and have frequent opportunity to speak to them; that churches and other faith institutions are deeply rooted in their communities; that they often run health and social service infrastructure; that faith and religious values are critical to responding to the pandemic – values of equity, of giving (both financial and in kind), of helping our neighbours, strangers and all in need.
The community of practice has been working on resources to help faith leaders communicate clearly and accurately with the communities they serve. The two companion pieces use the materials created.
Before looking at the common questions and concerns people across the world are voicing about the vaccines, we look at the significant role and opportunities faith leaders have to address these questions and concerns and support vaccine roll out.
What can faith leaders do to support vaccine roll out?
Faith leaders can play a significant role in vaccine preparedness, delivery, and advocacy for equity by:
- Making public statements (written or spoken) in support of Covid-19 vaccine uptake and calling for public health measures informed by the best scientific evidence.
- Posting accurate information on social media and web sites which is informed by the best scientific evidence about Covid-19 and vaccines.
- Answering questions and addressing common concerns honestly, using – and pointing to – accurate information sources; calling out obvious attempts to mis-inform or mislead people as wrong.
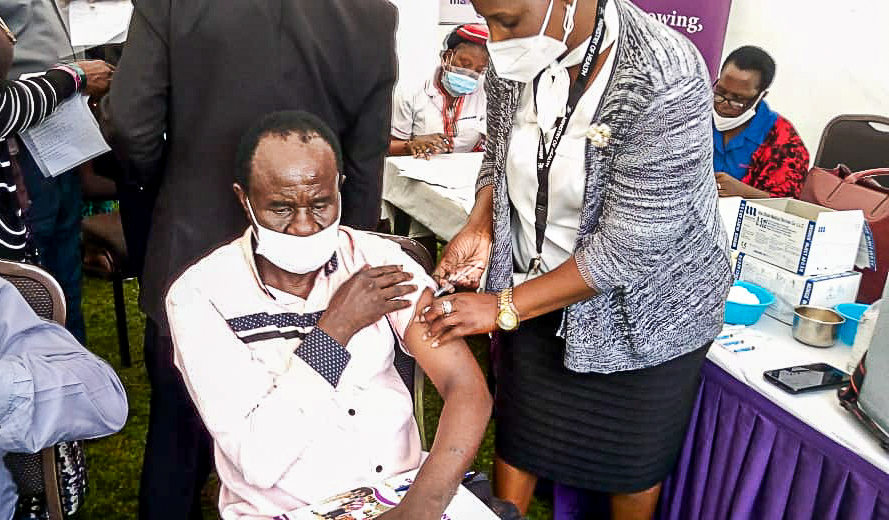
- Taking a photograph when you as a religious leader receive the vaccine and posting this on public media with a supportive statement on vaccine equity and uptake.
- Integrating Covid-19 responses and advocacy into your social infrastructure, such as schools, hospitals, clinics and social outreach programmes.
- Offering houses of worship, schools, hospitals, and clinics to be used for the national Covid-19 responses and as vaccination centres where appropriate. In some cases houses of worship can be used as ‘no questions asked’ vaccine centres in situations where undocumented migrants and others can receive vaccines.
- Enabling some of the existing religious financial giving to go towards Covid-19 care and support or to mechanisms that enable vaccine purchase and equitable distribution globally (or locally where marginalised communities are excluded from roll outs).
General Frequently Asked Questions about vaccines and COVID-19 vaccines
You can download this section as a pdf here
- How do vaccines work?
-
- A vaccine trains your immune system to fight infection, exactly like it would if you were exposed to a certain virus or bacteria. After getting vaccinated, you develop immunity to that disease, which means you can fight off the real virus if you come into contact with it.
- Vaccines are like putting on a seatbelt when you get in the car. The seatbelt keeps you safe if you should get in an accident. Vaccines keep you safe if you are exposed to a virus.
- Why are vaccines important?
-
- Vaccines are one of the most effective public health tools known to humankind and have saved the lives of millions of people from diseases such as smallpox, polio, measles, and many more.
- Vaccines are special because unlike most medicines, which treat or cure diseases, vaccines prevent them.
- Vaccines are a necessary tool to help end the pandemic.
- Would natural immunity protect me better than the COVID-19 vaccine?
-
- Getting the virus may offer some immunity, but we don’t know how long this protection lasts. If you contract COVID-19 naturally you may become very ill, have long-lasting health effects and possibly risk death. By taking the vaccine you are less likely to become seriously ill.
- The risk of severe illness and death from COVID-19 is far greater than any benefits of natural immunity, especially because the COVID-19 vaccine will help protect you without the risk of severe illness.
- How do we know the COVID-19 vaccine is safe?
-
- All vaccines are rigorously tested for safety and effectiveness. There were no serious safety concerns in the clinical trials for the vaccines. WHO certifies vaccines safe after a lengthy review process.
- WHO works closely with national authorities to ensure that global norms and standards are developed and implemented to assess the quality, safety and efficacy of vaccines.
- This is why WHO has a rigorous qualification process, manufacturers are required to submit a full set of data on their vaccine development, methods and results of testing and an independent committee of scientific experts review the data before the vaccine is qualified.
- You may have temporary reactions like a sore arm, headache, or feeling tired and achy for a day or two, but this is normal.
- All vaccines are rigorously tested for safety and effectiveness. There were no serious safety concerns in the clinical trials for the vaccines. WHO certifies vaccines safe after a lengthy review process.
- How was the COVID-19 vaccine developed so quickly?
-
- Scientists didn’t have to start from scratch. COVID-19 vaccines are built on decades of research and work developing vaccines for similar viruses.
- People working on the vaccine from around the world shared information with one another and thousands volunteered in clinical trials. All of this helped speed up the process.
- Were any shortcuts taken to develop the vaccine so quickly?
-
- There are many steps in vaccine development including studies before and during the three stages of clinical trials. During normal vaccine development these steps usually happen one after the other. To speed up the process to develop the COVID- 19 vaccine, some of these stages overlapped – but each individual stage was still completed and fully monitored.
- Even after a vaccine is approved and licensed it is continuously monitored. If anyone feels sick or has complications after being vaccinated, also known as adverse effects, these are reported immediately so that any changes that could be needed are made.
- Does the COVID-19 vaccine have side effects?
-
- You may have temporary reactions like a sore arm, headache or feel tired and achy for a day or two after receiving the vaccine. This means your body’s immune response is working. These side effects are not serious or long-lasting.
- If anyone feels sick or has serious complications after being vaccinated, also known as adverse effects, these are reported immediately so that vaccine safety is continuously checked.
- Why was the COVID-19 vaccine developed so quickly when it takes years for other vaccines to be made?
-
- COVID-19 was declared a Public Health Emergency of International Concern on January 30th. COVID-19 has affected the health, economy and social fabric of every country and community globally. Due to the scale of the pandemic, researchers and scientists from around the world have come together to share resources and knowledge to find a safe and effective vaccine as quickly as possible. A vaccine is an important tool towards ending the pandemic.
- Imagine working on a puzzle on your own for many days. Now imagine how fast you would complete the same puzzle if you had the help of ten friends!
- What’s the difference between the different vaccines?
-
- All vaccines activate your immune system, so you are ready to fight off COVID-19 if you come into contact with it. Some vaccines mimic the virus, while others use a weakened or killed germ – none of these vaccine types can make you sick with COVID-19. Instead, the vaccines teach our bodies to recognise COVID-19 so you won’t develop severe disease if you contract the virus. Read more about the different types of vaccines here.
- Can you be infected with COVID-19 from the vaccine?
-
- You cannot get COVID-19 from the vaccine nor will the COVID-19 vaccine cause you to test positive on COVID-19 tests.
- You may have temporary reactions like a sore arm, headache or feeling tired and achy for a day or two after receiving the vaccine.
- For how long will the vaccine protect me from COVID-19?
-
- Since the trials for each licensed vaccine have just ended, we know that the vaccines protect people from COVID-19 for at least two months. As time goes on people will be vaccinated for a longer period of time and we will continue to measure how long immunity from the vaccine lasts. It is possible that COVID-19 vaccines will be needed yearly, like the flu shot.
- Are two doses of COVID-19 vaccine necessary?
-
- The Pfizer and Moderna vaccines require two shots to build up strong immunity against COVID-19. The vaccines provide their full protection from COVID-19 two weeks after receiving the second dose. Other vaccines, such as the measles, mumps and rubella vaccine also require more than one dose.
- COVID-19 vaccines being tested or reviewed now use single or multiple doses. The number of doses a vaccine requires depends on the type of vaccine. Read more about the different types of vaccines here.
- Who will be vaccinated first?
-
- To save lives higher risk groups like health workers and older adults may be the first recipients. Contact your local health authority to confirm the planned vaccine rollout in your community.
- What should you do after you have been vaccinated?
-
- The COVID-19 vaccine protects you from becoming seriously ill with the disease, but you may still be able to pass the virus to others. So, it’s important to continue practicing physical distancing, frequently clean your hands, wear a mask, and follow the advice of your local health authority.
- Do I need to get vaccinated if everyone around me already is?
-
- The vaccine protects you from developing severe disease, which means you are less likely to require hospitalisation or medical support. This benefits your health and also reduces the burden on the healthcare system.
- Can we stop physical distancing, mask wearing and other measures once we have been vaccinated?
-
- Even if you are vaccinated, you should still frequently clean your hands, maintain physical distance and wear your mask to help keep everyone safe. This is because we don’t know yet if the vaccines prevent transmission, we only know for sure that they significantly reduce the risk of serious illness. Until the majority of people are vaccinated, we need to assume we can still spread the virus. When more data on the impact of vaccines on transmission will become available, we will update these recommendations.
For more information: Vaccination & Immunization FAQs on WHO’s website